feature
Current Treatment of Ocular Rosacea
Topical cyclosporine proves to be effective
in treating rosacea.
BY
BARRY A. SCHECHTER, M.D.
Rosacea is a chronic cutaneous inflammatory condition, which affects the eye in a significant proportion of cases. The pathogenesis of the disease has never been fully identified although changes in the inflammatory response have been suspected. Ocular rosacea affects the eyelid margins and the meibomian glands. Lid margin telangiectasia, meibomian gland inflammation and inspissation1 with subsequent tear film abnormalities leads to a destabilized tear lipid layer, which may result in increased tear evaporation.
Patients' ocular surface signs and symptoms are sometimes consistent with those of keratoconjunctivitis sicca (KCS). Overexpressed inflammatory markers and cytokines were noted by several investigators.2,4 Pisella and colleagues, found a decreased number of goblet cells. Other researchers found elevated levels of matrix metalloproteases (MMPs).3,5 Typical findings on an examination are decreased tear break-up time, conjunctival hyperemia, foreign body sensation and ocular discomfort.1,4
|
|
|
Figure 1. Patient with significant ocular surface pathology due to ocular Rosacea. |
Treatments
Traditional treatments for ocular signs and symptoms of rosacea have included warm soaks and lid scrubs when debris or discharge is associated. Oral tetracyclines are sometimes utilized, but their beneficial action appears distinct from any potential antibacterial activity. Tetracyclines have been known to inhibit the expression of MMPs.5
If a concomitant lid margin infection is present, topical antibiotics are utilized in the form of ointments or drops. Topical corticosteroids may be used in a pulsed fashion to bring severe inflammation under control, although their use has many potential side effects if used chronically.
Artificial tears have long been used for chronic management of dry-eye symptoms. However, these drops provide insufficient long-term symptomatic relief in most patients and fail to address the underlying pathology.
Topical cyclosporine (Restasis, Allergan Inc., Irvine, Calif.) has been shown to increase tear production and improve the quality of naturally produced tears and is the first approved therapeutic agent for the treatment of chronic dry eye.6 Topical cyclosporine has also been shown to significantly suppress the number of activated T lymphocytes within the conjunctiva, reducing the ocular inflammatory response.6
Case Study
|
|
| Figure 2. Patient after 8 weeks of treatment with topical cyclosporine. |
A 42-year-old male who worked as a salesman presented to my office complaining of intermittent foreign-body sensation and discharge. He stated that his eyes had been "red for as long as he could remember." He confided that he often had to use over-the-counter (OTC) eye drops "to get the red out" before meeting with clients or upper management. He rarely drank alcohol, feeling that this exacerbated the redness and irritation of his eyes, as well as making his nose and cheeks flush. The only medication he used was Lipitor to control his hypercholesterolemia.
His facial appearance was ruddy with telangectasia evident at the tip of the nose, the malar area and the eyelid margins. His visual acuity (VA) fluctuated slightly between blinks but measured 20/25.
Slitlamp examination was significant for scurf and dried discharge on the eyelashes, eyelid margin telangiectasia, meibomian gland inspissation and notching of the lid margins. Conjunctival hyperemia between the palpebral fissures with injection near the caruncle was noted (Figure 1). Tear break up time (TBUT) measured 2 seconds with a Schirmer score (anesthetized) of 4 mm OD and 5 mm OS. The remainder of his ocular examination was unremarkable.
The patient was started on a course of topical gatifloxacin 0.3% ophthalmic solution q.i.d., and fluorometholone 0.1% ophthalmic solution b.i.d. After 1 week, when the discharge was improved, he began topical cyclosporine b.i.d., discontinued gatifloxacin, and tapered the fluorometholone over a week. Eight weeks later, the conjunctival hyperemia was significantly reduced (Figure 2), TBUT measured 8 seconds OU and his Schirmer scores were 10 mm and 12 mm.
Six months later, the patient is comfortable, rarely feels the need to use OTC tear drops and feels that he sees better while continuing the topical cyclosporine.
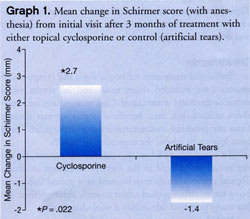
In a poster at ARVO in 2005,11 which has been subsequently accepted for publication, I discussed a study which compared the efficacy of cyclosporine ophthalmic emulsion 0.05% with an artificial tear solution (Refresh Plus, Allergan Inc., Irvine, Calif.) used as a control, for the treatment of rosacea-associated eyelid and corneal pathology.
The study was a double-masked, prospective trial following 37 patients with rosacea-associated eyelid and corneal changes. Patients were enrolled after any active infections were treated with lid scrubs and topical antibiotics. Patients were then randomized to cyclosporine or artificial tears for 3 months. All patients were withdrawn from oral doxycycline for at least 2 weeks prior to study entry, and patients with eyelid defects or lagophthalmos were excluded.
Topical cyclosporine provided statistically significantly greater improvements in Schirmer scores (Graph 1), TBUT (Graph 2), corneal staining and ocular surface disease index (OSDI) scores (Graph 3) compared to artificial tears solution after 3 months of treatment. Cyclosporine produced a statistically significant increase in Schirmer (with anesthesia) scores of 2.7 mm + 2.2 mm after 3 months of treatment (P<0.001). Conversely, Schirmer scores worsened in the artificial tears group, with a mean decrease of 1.4 + 4.6 mm (P=0.271). Similarly, the mean TBUT score significantly improved in the cyclosporine-treated patients (a mean increase of 3.56 + 1.5 seconds, P<0.001), but worsened in the control group (a mean decrease of 0.04 + 1.6 seconds, P=0.929). Cyclosporine-treated patients exhibited a significantly greater mean reduction in corneal staining (-1.3 + 0.53) compared with artificial tears (-0.2 + 0.83) after 3 months of treatment (P<0.001).
Moreover, cyclosporine provided significantly greater improvement in OSDI scores than did artificial tears (mean reduction of 11.5 + 8.8 with cyclosporine vs. a mean decrease of 2.9 + 11.6 with tears, P=0.022).
In this study, cyclosporine provided statistically significant improvements in Schirmer scores, OSDI, TBUT and corneal staining scores when compared to artificial tears. This is most likely due to the effects cyclosporine has on increasing tear production and decreasing inflammation.6 The ability of cyclosporine to significantly improve these scores may be due to a cyclosporine-mediated reduction in the number of activated lymphocytes within the conjunctiva.7 By reducing activated lymphocytes and increasing tear production, cyclosporine decreases inflammation within the eye and improves patient signs and symptoms.
The anti-inflammatory mechanisms of
cyclosporine are highly appropriate for the treatment of ocular rosacea, as the
condition has been shown to have an inflammatory etiology. Barton and associates
conducted a study comparing tear fluid concentrations of interleukin-1alpha (IL-1alpha)
and tumor necrosis factor-alpha (TNF-alpha) in ocular rosacea with those in control
subjects.2 Tear turnover was lower in
patients with rosacea than in controls, and Schirmer scores were also statistically
lower in patients with rosacea than in controls.
After 6 months of use, topical
cyclosporine was shown to decrease inflammatory cytokines in the conjunctival epithelium
of dry eye patients with increased tear production.8

Despite the relatively common incidence of ocular rosacea, the diagnosis is routinely missed by ophthalmologists or, when it is made, is often undertreated. A recent evaluation by Akpek and associates reported that the most common symptoms recorded in a cohort of 131 patients with ocular rosacea included foreign-body sensation and burning, and the most common signs were telangiectasia and irregularity of lid margins and meibomian gland dysfunction.1 The nonspecific nature of these signs and symptoms likely contributes to the possibility of misdiagnosis. However, this same report underscores the potential consequences of undertreating ocular rosacea. Although the majority of patients (86.3%, 113/131) studied received oral tetracyclines, the standard of care for rosacea, 13 of them had decreased VA at the time of presentation due to corneal complications. Six of these patients required penetrating keratoplasty during the course of their disease. Seven patients had severe cicatrizing conjunctivitis at the time of referral and seven patients were left with VA of <20/400. Alarmingly, one patient even underwent enucleation for corneal perforation and endophthalmitis.1
A prior report by Zengin and associates also found a strong correlation between rosacea and meibomian gland disease.9 In that study, patients with poor meibum secretion and inspissation exhibited tear film instability and experienced premature tear evaporation.
The finding that cyclosporine is an effective treatment for the signs and symptoms of ocular rosacea is consistent with another recent evaluation.10 Perry and associates reported that topical cyclosporine was effective in treating ocular rosacea patients unresponsive to standard therapy. Moreover, most patients in that cohort (71%) were able to discontinue all other medications.10 These authors also found that topical cyclosporine was safe and well tolerated in patients with ocular rosacea.

followed an average of 5.2 months
(range 2 to 119 patients). Nine patients (16%) did not respond and withdrew. Twenty-one
patients (38%) reported mild-to-moderate relief of symptoms with improvement in
clinical exam. Twenty-five patients (46%) had significant improvement or complete
resolution. At long-term follow-up, 18 (39%) required no additional medications
and 30 (65%) were still taking low-dose tetracycline. Wittpenn concluded that topical
cyclosporine is efficacious in treating ocular rosacea.10
Given the excellent side effect profile of topical cyclosporine and its lack of systemic absorption, ophthalmologists should consider utilizing topical cyclosporine in the treatment of patients with ocular rosacea.
Dr. Schechter is the director of Department of Cornea and External Disease, Florida Eye Microsurgical Institute, Boynton Beach, Fla. His practice involves the treatment of disorders of the ocular surface, and cataract and refractive surgery. He can be reached at BDSCH77@aol.com or (561)737.5500.
References
1. Akpek EK, Merchant A, Pinar V, Foster CS. Ocular rosacea: patient characteristics and follow-up. Ophthalmology. 1997;104:1863-1867.
2. Barton K, Monroy DC, Nava A, Pflugfelder SC. Inflammatory cytokines in the tears of patients with ocular rosacea. Ophthalmology. 1997;104:1868-1874.
3. Afonso AA, Sobrin L, Monroy DC, Selzer M, Lokeshwar B, Pflugfelder SC. Tear fluid gelatinase B activity correlates with IL-1alpha concentration and fluorescein clearance in ocular rosacea. Invest Ophthalmol Vis Sci. 1999;40:2506-2512.
4. Pisella PJ, Brignole F, Debbasch C, Lozato PA, Creuzot-Garcher C, Bara J, Saiag P, Warnet JM, Baudouin C. Flow cytometric analysis of conjunctival epithelium in ocular rosacea and keratoconjunctivitis sicca. Ophthalmology. 2000;107:1841-1849.
5. Sobrin L, Liu Z, Monroy DC, Solomon A, Selzer MG, Lokeshwar BL, Pflugfelder SC. Regulation of MMP-9 activity in human tear fluid and corneal epithelial culture supernatant. Invest Ophthalmol Vis Sci. 2000;41:1703-1709.
6. Sall K, Stevenson OD, Mundorf TK, Reis BL. Two multicenter, randomized studies of the efficacy and safety of cyclosporine ophthalmic emulsion in moderate to severe dry eye disease. CsA Phase 3 Study Group. Ophthalmology. 2000;107:631-639.
7. Kunert KS, Tisdale AS, Stern ME, Smith JA, Gipson IK. Analysis of topical cyclosporine treatment of patients with dry eye syndrome: effect on conjunctival lymphocytes. Arch Ophthalmol. 2000;118:1489-1496.
8. Turner K, Pflugfelder SC, Ji Z, Feuer WJ, Stern M, Reis BL. Interleukin-6 levels in the conjunctival epithelium of patients with dry eye disease treated with cyclosporine ophthalmic emulsion. Cornea. 2000;19:492-496.
9. Zengin N, Tol H, Gunduz K, Okudan S, Balevi S, Engodru H.. Meibomian gland dysfunction and tear film abnormalities in rosacea. Cornea. 1995;14:144-146.
10. Perry HD, Wittpenn JR, D'Aversa G, Donnenfeld ED. Topical cyclosporine 0.05% for the treatment of chronic, active ocular rosacea. Presented at: the Annual Meeting of the Association for Research in Vision and Ophthalmology (ARVO); May 1-5, 2005; Fort Lauderdale, Fla.
11. Schechter BA,Wittpenn JR Efficacy of Topical Cyclosporine for the Treatment of Ocular Rosacea. Presented at: the Annual Meeting of the Association for Research in Vision and Ophthalmology (ARVO); May 1-5, 2005; Fort Lauderdale, Fla.










