Point Counterpoint
Two surgeons were
asked to provide commentary on their use of two technologies
to create a flap
prior to LASIK: the mechanical microkeratome and the femtosecond laser.
These
physicians explain what they believe to be the benefits of the individual technology
they are utilizing and detail some of the limitations of the other technology.
The Time is Now to Switch to All-Laser LASIK
The
increased safety and efficacy of IntraLase adds value for our patients and practice.
BY ELIZABETH A. DAVIS, M.D.
At our practice, we pride ourselves on being at the forefront of patient care. In fact, we work to be on the cutting-edge of the ophthalmic field. Yet, when it came to moving to an all-laser LASIK procedure, we were actually among the naysayers about the technology.
It was not until we saw some credible data about the femtosecond laser (IntraLase, Irvine, Calif.) that showed improved safety and efficacy that we started to change our minds. Now, we could not be bigger fans. Here are some factors we considered when purchasing an IntraLase, and why today, I believe it brings added value for our patients and our practice.
Improved Visual Outcomes
Our first laser was the 15 kHz model. With that laser, we did see some delay in visual acuity (VA) recovery to corneal edema. However, when we upgraded to the 30 kHz laser, we compared outcomes to a mechanical microkeratome (MM), and we saw a trend toward better VA in the IntraLase eyes. We now have the 60 kHz laser, and initial results have shown even better outcomes. The flap created with the 60 kHz laser is done in the same time it takes to create a MM flap (20 seconds). The lift is easier, and the bed quality is outstanding. Postoperatively, there is no visible flap edema and the flap edges are difficult to see. Visual recovery is even faster and there is no increased incidence of inflammation.
We do not yet understand why there is this improvement in VA compared to the MM, but we believe it has to do with the quality of the flap bed created by the laser.
|
|
|
Dr. Davis converted to the IntraLase femtosecond laser. |
Complication Rates and Safety
Here, we looked at the following points to determine which option provided lower complication rates and improved safety for our patients:
►Diffuse Lamellar Keratitis(DLK)/photophobia. On this point, the MM and the laser proved equal. It is important to note, we saw none of the DLK or transient light sensitivity that was reported with early usage of the IntraLase. With an increase in the repetition rate and the lower energy levels, this should really become a thing of the past.
►Slipped flap or microstria. The advantage goes to IntraLase, as we did not see a single case of this in our study.
►Epithelial defects and epithelial ingrowth. Again, IntraLase proves superior because there is little risk of epithelial defects with the applanation cone of an Intralase. In the past, I would have been hesitant to do LASIK in a patient with anterior basement membrane dystrophy with a MM because of the frictional translational force across the corneal surface. However, I am comfortable performing this procedure with the IntraLase.
►Corneal steepness. One does not need to be concerned with this when using IntraLase since applanation occurs in a vertical rather than translational fashion. Buttonholes and free flaps due to excessively steep or flat corneas are therefore not a concern. In terms of improved safety, we found a number of benefits. Most importantly, the surgeon can visualize the flap as it is created; with the majority of MMs, the surgeon has no visibility.
With the IntraLase laser, the surgeon knows what the flap is going to look like — if it is centered and if it is large enough. If the size or centration is not acceptable, applanation can be reapplied. This is impossible to do with the MM. Also, there is no concern about partial flaps with the laser. With the MM, a partial flap means stopping the procedure and sending the patient home for 3 to 6 months to heal before attempting LASIK again. This can make the patient nervous and reduce the surgeon's credibility.
With the IntraLase, if suction is lost and only a partial raster pattern is created, then suction can be reapplied immediately and flap creation started over. This is particularly reassuring in patients at higher risk for suction loss, such as those with tight orbits or deep sockets.
|
|
|
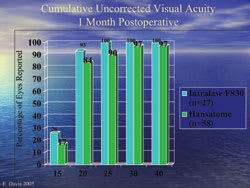
This table shows 1-month visual outcomes in our initial study with the 15 kHz femtosecond laser. |
We can now include a wider range of patients for LASIK. Previously, I would have considered PRK in patients with thinner corneas. However, I can set the laser for a really thin flap, so I consider LASIK in these patients. The ability to place the hinge in any location, allows LASIK to be safely performed in patients with pteyrgium without concern for cutting through this fibrovascular growth.
Practice Income
There is an additional cost to an IntraLase procedure compared to the MM. In our practice, this works out to approximately $70 to $80 per case. This is a cost that can be appropriately passed on to the patient. Currently, we have factored in a modest amount of profit for all-laser LASIK compared to MM LASIK. Initially, we were quite concerned about how the IntraLase laser would impact patient flow. Our typical schedule was to treat two patients, or four eyes, every hour and I thought using the laser might hinder that. Fortunately, it has not been the case. With the 60 kHz laser, it only takes about 3 to 4 more minutes for a bilateral case with the IntraLase compared to the MM. We have the IntraLase and excimer laser in the same room next to each other and swing the patient bed between the two lasers.
Happy Patients = Happy Staff
We have certainly seen an increasing interest in IntraLase. Now close to 90% of our referring doctors and patients are choosing IntraLase in the center where we provide this technology. Here is the one point that I believe makes the IntraLase a standout success — patients and surgeons are generally happier with the all-laser procedure. Many of our patients now come in asking for it. They find the idea of a laser-created flap to be more palatable than the MM. In turn, they are often more relaxed during surgery. Relaxed patients make for relaxed staff and surgeons. Some may maintain that the majority of patients are not even aware that a metal blade is typically used to create the flap. I have found the opposite to be true — most are fully aware, and it is that very aspect of surgery that can frighten them the most.
From Skeptics to Advocates
I now use the IntraLase laser in 90% or more of my LASIK cases at that one center. We have gone from skeptics to big fans. If we were in the position to do so, we would have one at all five of our laser centers.
Dr. Davis is a consultant for Bausch & Lomb and IntraLase. She is a partner of Minnesota Eye Consultants and is an assistant clinical professor of Ophthalmology at the University of Minnesota.Dr. Davis can be e-mailed at eadavis@mneye.com.
Mechanical Microkeratomes: A
Safe, Reliable, Mature Technology
Improved microkeratomes are making the most challenging part of LASIK simpler and safer.
BY
Y. RALPH CHU, M.D.
Using the latest generation of mechanical microkeratomes (MM) gives me peace of mind. Over the years, microkeratome technology has evolved in its safety for patients, predictability in flap creation and simplicity of use. Having an instrument you are comfortable with that makes safe, effective flaps is part of providing patients with a high level of quality care. There are several reasons why I am continuing to use a MM and I will lay them out in this article.
|
|
| According to Dr. Chu, using the refined technology of mechanical microkeratomes to create flaps results in a high quality of care for his LASIK patients. |
The Technology's Evolution
The safety and consistency in MMs has evolved and continuously helped surgeons meet their intraoperative needs by creating safe, viable flaps for LASIK patients. Features such as automated suction, computerized safety checks and electronic voice confirmations informing the surgeon he or she can proceed with the procedure are improvements that make the most challenging part of LASIK simpler.
And the technology has progressed to the point that my microkeratome, the Amadeus II (Advanced Medical Optics, Santa Ana, Calif.), now has the ability to make Epi-LASIK flaps. This has allowed patients who previously may not have been the best candidates for LASIK to undergo a modern surface ablation procedure instead.
Patients with dry eye, thin corneas, mildly asymmetrical astigmatism or anterior basement membrane corneal dystrophy, are candidates for Epi-LASIK. This "two-in-one" capability has improved safety for patients.
This has helped to increase my patient base for laser vision correction procedures overall. While I still perform LASIK on approximately 85% to 90% of my laser correction patients, the other 10% to 15% are surface ablation — and this number is growing. My microkeratome can be fitted for a LASIK procedure or switched for epi-LASIK on the same unit in moments and the transition is seamless.
One area of recent debate has been the development of thin-flap LASIK. Some are saying that by utilizing the femtosecond laser, surgeons can create a thinner flap than the MM and avoid some of the potential complications associated with creating thicker flaps. However, I would argue that whether a flap is thick or thin, the creation of a flap is still a surgical incision, and therefore, still has the potential for complications such as dry eye or ectasia. If there is any concern about creating a flap, then I believe surface ablation should be performed. I think thin-flap LASIK should be no-flap LASIK.
Femtosecond vs. Mechanical
In head-to-head comparison studies between mechanical microkeratomes and the femtosecond laser there have been conflicting results about which technology is favorable for use in LASIK. Some study results favor the femtosecond laser while others favor the mechanical microkeratome. Many studies have shown similar visual acuity results between the two types of microkeratome. Flap thickness variations and complication rates were also similar between the two devices across several studies.
There are two areas, nonetheless, where the MM has advantages over the femtosecond laser. It takes longer to create a flap utilizing the femtosecond laser, and it is a more expensive procedure overall.
I will acknowledge that having "all-laser LASIK" may create some initial buzz around your practice, but with patients paying out of pocket for the additional costs of the femtosecond laser — which could be hundreds of dollars more per procedure depending on the volume of your practice — this could discourage some potential patients.
Safety is a critical concern of all LASIK surgeons. Any surgical procedure has potential complications. The creation of a lamellar flap is a surgical procedure and has certain risks whether the flap is made with a laser or a blade. I think that the complications between two different devices may also be different, but to infer that a laser device is complication free is implausible. Complications such as ectasia, buttonholes and DLK are risks with both femtosecond and mechanical microkeratomes. Others, such as transient light sensitivity, are specific to the femtosecond microkeratome.
Treating the Ocular Surface
An area that I believe has helped to make LASIK an even more successful procedure is the understanding that the health of the ocular surface is critical to the quality of vision. Adoption of a comprehensive treatment regimen of the ocular surface throughout a patient's surgical experience helps to improve patient outcomes. A healthy, moist ocular surface allows me to get good refractions, leads to accurate wavescans, helps create viable flaps and provides an environment that minimizes inflammation thus allowing the cornea to heal faster.
As such, I begin a pharmacological regimen before a patient undergoes LASIK. I have all patients use artificial non-preservative tears q.i.d. 2 for weeks before surgery. These patients also begin Restasis (cyclosporine 0.05%, Allergan) treatment b.i.d. for 2 weeks prior to surgery and as long as 3 to 6 months after LASIK. Lastly, I will also prescribe a fourth generation fluoroquinolone antibiotic q.i.d. for 3 days before and for 4 days after surgery.
Mechanical Microkeratomes Deliver
Mechanical microkeratomes have evolved in their safety, predictability and simplicity in creating lamellar flaps for the LASIK procedure. And, with the increased use of surface ablation procedures thru Epi-LASIK, having a device that can create both lamellar and epithelial flaps is not only convenient but also critical.
From my perspective, this raises the bar for new technologies such as the femtosecond laser as they enter the microkeratome market.
Dr. Chu is a consultant for AMO. He is the founder and medical director of the Chu Vision Institute in Edina, Minn. He can be e-mailed at yrchu@chuvision.com.