Corneal clarity dictates much of a patient’s vision, yet etiologies such as infection, inflammation, and trauma can contribute to corneal scarring that obstructs vision. The challenge in anterior corneal scarring is the decision of whether to perform transplant surgery, due to its risk of complications.
Fortunately, there are several alternatives to transplant in eyes with cornea scarring, along with several clinical factors to consider.
KEY TAKEAWAYS:
- Not all corneal scars require transplant
- Medical management should be the first-line treatment
- Scleral lenses may delay or eliminate the need for surgery
- Surgical options are layered by depth of involvement
- Full-thickness keratoplasty should be reserved for severe cases
Location of Pathology
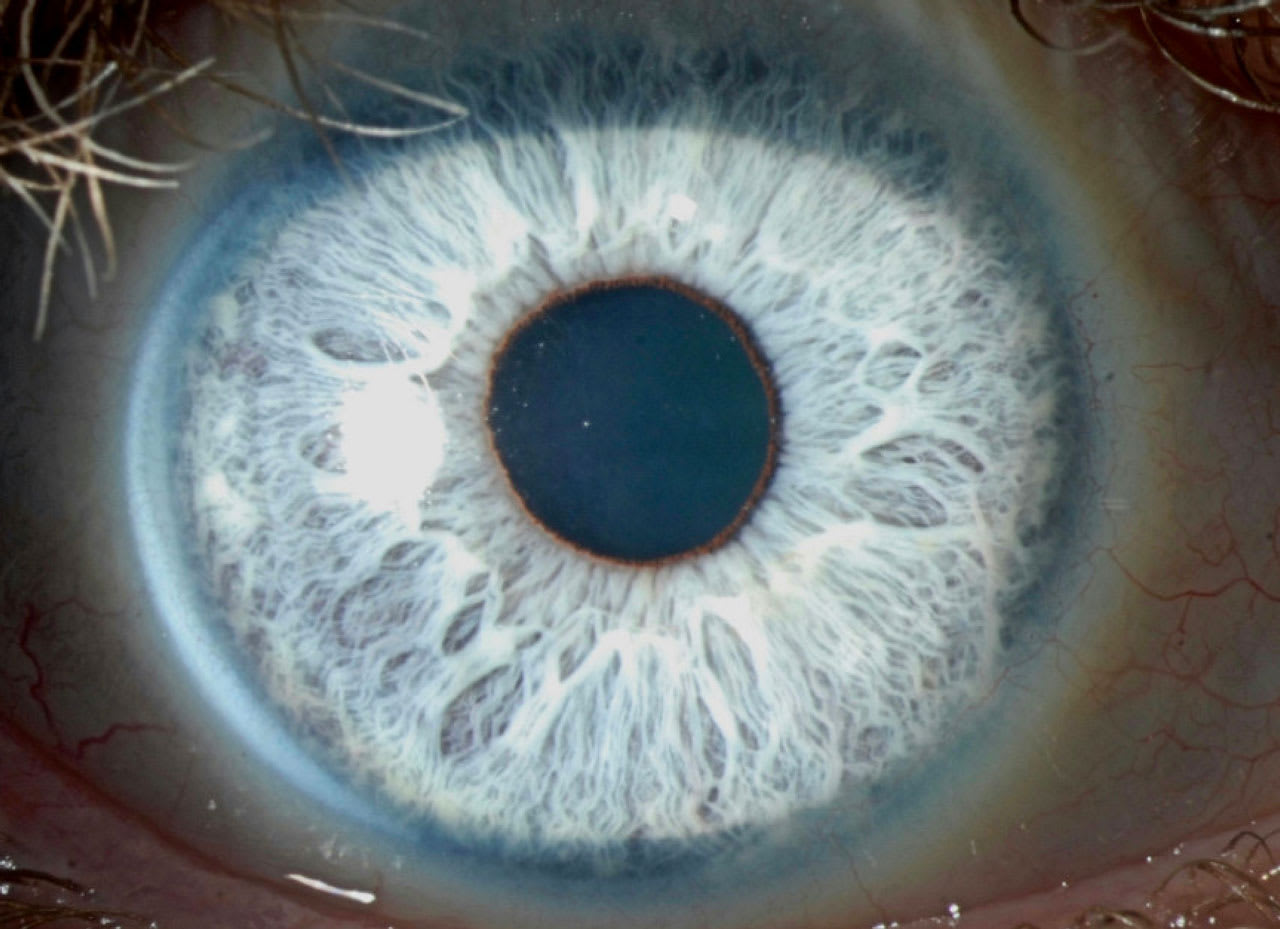
First, it is important to understand which corneal layers are most affected by the pathology. Superficial scarring that is limited to the anterior-most stroma often can resolve with time or with medical management, as discussed below. In addition, superficial keratectomy using a laser or a diamond burr can improve vision when limited to the anterior 15% to 20% of the cornea. Deeper scarring, on the other hand, may not improve with medical management and may need surgical intervention, such as an anterior keratoplasty or a full-thickness keratoplasty.
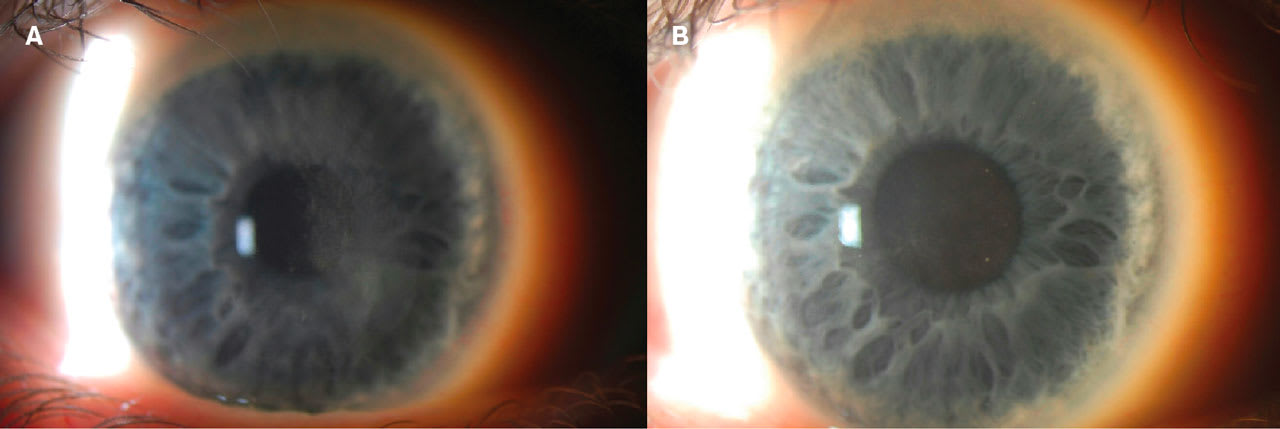
Location on the cornea also plays an important role in choosing treatment. Central scarring is the most visually impactful and creates an actual obscuration to vision, even if the patient tests well on the eye chart. However, for paracentral and more peripheral scarring, I’m often impressed by how much of the vision is decreased by irregular astigmatism rather than by true opacity. I send these patients for a scleral contact lens evaluation, and often they can achieve amazing results without surgery.1
Density of Scar
The choice of treatment should also be based on the degree of scarring. It’s often striking how much faint scarring can improve with time. I’ve seen anterior stromal scarring left by prior corneal ulcers fade and the patients’ vision improve. However, dense and deep scars often do not improve with time.
Medical Management
Medical management can always be considered prior to surgical treatment. Early in the time course, treatment with topical steroids can assist with some types of scarring, especially if the haze is still active. If the disorder is linked with active infection, always medically control any inflammation or infection. For cases like neurotrophic keratitis, the recombinant human nerve growth factor (rhNGF) cenegermin is used to close the stage 2 or 3 ulcer, but it has also been shown to improve the subepithelial haze that occurs from chronic epithelial defects.
For scars, topical losartan has been shown in a few limited studies to improve some types of cornea haze. The dose of 0.8mg/mL 6 times a day is recommend for 3 to 6 months.2 In our practice, we utilize scleral lenses to determine the patient’s best corrected visual acuity (BCVA); the scleral lens reservoir can serve as a means of delivering medication to the cornea, such as preservative-free dexamethasone 0.001% and plasma rich in growth factors (PRGF). The latter also has been shown to help with anterior cornea scarring. For this purpose, we use it without scleral lenses 4 times a day for 6 months.
Superficial Keratectomy
When medical management fails to improve vision, superficial keratectomy with a diamond burr can be used to treat very shallow anterior corneal pathology. It is important to understand how deep the pathology is and how to prevent recurrence of haze after treatment of the scar. I will use superficial keratectomy similarly for band keratopathy with ethylene diamine tetra-acetic acid (EDTA) chelation, especially when there is haze underlying the calcium deposits.
For deeper haze, we utilize phototherapeutic keratectomy (PTK) by first removing the epithelium, then using the laser to deliver broad spot sizes and ablating the area of anterior cornea haze.3 It is important to use mitomycin following these treatments to prevent recurrence of haze.4 Anterior segment imaging can assist in understanding the depth of the haze, and the laser can be programmed for the appropriate number of microns of ablation. It is important that patients understand that when treating anterior cornea pathology there is a chance of a hyperopic shift due to flattening of the cornea.
Anterior Lamellar Keratoplasty
Deeper haze and scarring will require keratoplasty. While keratoplasty is an effective surgery, there is a lifelong chance of rejection, especially with a full-thickness transplant. An anterior lamellar keratoplasty (ALK) can assist with reducing that risk. Performing an ALK and estimating the depth of pathology is one way to approach these cases. However, 2 challenges arise: interface irregular astigmatism and interface haze.
Deep Anterior Lamellar Keratoplasty
A deep anterior lamellar keratoplasty (DALK) can provide clarity to the anterior cornea and reduce interface haze and astigmatism compared to ALK. Several techniques are utilized to achieve the perfect depth of stroma removal, including the big bubble technique and the newer “grip-and-rip” technique. Even with perfect surgery, there could be some reduction in BCVA and contrast.5 However, the risk of graft rejection is reduced, which is key for patients—especially those who are younger or at higher risk for complications.
Full-Thickness Keratoplasty
Lastly, a full-thickness keratoplasty is always an option for patients with corneal pathology. This can be used even in the setting of a DALK when the above techniques do not work well and conversion to full-thickness penetrating keratoplasty (PKP) is best. In addition, I use a full-thickness PKP for patients whose disease has also caused endothelial dysfunction.
In summary, cornea scarring is important to address to allow for the patient’s best vision. Medical management is an important first step. Scleral contact lenses can help to rehabilitate vision while also providing a way to deliver medication to the cornea to treat haze. Lastly, surgical options like superficial keratectomy and keratoplasty can greatly help patients and their vision. OM
References
1. Parra AS, Roth BM, Nguyen TM, Wang L, Pflugfelder SC, Al-Mohtaseb Z. Assessment of the Prosthetic Replacement of Ocular Surface Ecosystem (PROSE) scleral lens on visual acuity for corneal irregularity and ocular surface disease. Ocul Surf. 2018;16(2):254-258. doi:10.1016/j.jtos.2018.01.003
2. Dutra BAL, Wilson SE. Topical Losartan in the Management of Corneal Scarring Fibrosis: Update on Dosage, Efficacy, and Potential Epithelial Toxicity. J Ocul Pharmacol Ther. Published online April 16, 2025. doi:10.1089/jop.2024.0200
3. Rush SW, Han DY, Rush RB. Optical coherence tomography-guided transepithelial phototherapeutic keratectomy for the treatment of anterior corneal scarring. Am J Ophthalmol. 2013;156(6):1088-1094. doi:10.1016/j.ajo.2013.06.026
4. Porges Y, Ben-Haim O, Hirsh A, Levinger S. Phototherapeutic keratectomy with mitomycin C for corneal haze following photorefractive keratectomy for myopia. J Refract Surg. 2003;19(1):40-43. doi:10.3928/1081-597X-20030101-08









